

(732) 238-3773
CSS3 Menu Button by Css3Menu.com
Diptika Patel, M.D.

 |
|
|||
 |
Call us now: (732) 238-3773 |
|
||
|
|
CSS3 Menu Button by Css3Menu.com |
|
||
|
Puneet Sahgal, M.D., F.A.C.C. Diptika Patel, M.D. |
 |
|
||
|
|
FREQUENTLY ASKED QUESTIONS |
|
||
|
|
 GENERAL QUESTIONS
What kind of doctor is Dr. Sahgal?
Dr. Sahgal is a primary care/internal medicine physician, and specializes in cardiology and vein disease, with extensive experience in these fields.
GENERAL QUESTIONS
What kind of doctor is Dr. Sahgal?
Dr. Sahgal is a primary care/internal medicine physician, and specializes in cardiology and vein disease, with extensive experience in these fields.Can Dr. Sahgal be my primary care doctor? Yes, Dr. Sahgal is Board Certified in Internal Medicine and listed as a PCP (primary care physician) with most of the insurance plans. We provide all Primary Care Services. Our staff will assist you with questions related to your insurance plan. Can Dr. Sahgal be my Primary Care Doctor as well as my Cardiologist? Yes, Dr. Sahgal is Board Certified in both Internal Medicine and Cardiology. A large number of patients in our practice have him as their Primary Care Physician and as their Cardiologist. Can Dr. Sahgal be my Cardiologist while I keep my own Primary Care Physician? Yes, Dr. Sahgal is Board Certified in Cardiovascular Diseases and is listed as a Cardiologist with almost all of the insurance plans. We provide all major Cardiology Services. Our practice will inform your PCP about your heart related testing and progress. What is Vein Care? Veincare involves evaluation, treatment and management of vein diseases and disorders. Painful varicose veins, spider veins and various other venous disorders are very common and under-recognized and under-treated. We provide all major Veincare Services and treatments. What insurance plans to you accept? We accept most insurance plans. For details please refer to the Insurances tab. Are you accepting new patients? Yes, we do accept new patients. You will be able to see the doctor within 24-48 hours. What hospitals is Dr. Sahgal affiliated with?
Do you have a blood drawing facility in your office? Yes, we have a phlebotomist in the office at all times. I am Dr. Sahgalís patient. How can I get my medications refilled? Your prescriptions will be promptly refilled as long as you are following Dr. Sahgal on a regular basis. Please call the office and we will call your pharmacy. Back to Top ELECTROCARDIOGRAM What is an Electrocardiogram? Electrocardiogram is a recording of electric activity of your heart. You will lay on a table. Certain areas of your arms, legs, and chest will be cleaned and may be shaved. Several electrodes are attached to the skin on each arm and leg and on your chest. These are hooked to a machine that traces your heart activity onto a paper. You will be asked to lay very still and breathe normally during the test. Sometimes you may be asked to hold your breath. You should not talk during the test. After the test, the electrode paste is wiped off. Test will take about 5-10 minutes. EKG is a safe test. The electrodes are used to transfer an image of your heart's electrical activity to the tracing on paper. No electricity passes through your body from the machine, and there is no danger of electrical shock. Back to Top ECHOCARDIOGRAM What is an Echocardiogram? An echocardiogram (echo) is a test that uses high frequency sound waves (ultrasound) to make pictures of your heart. The test is also called echocardiography or diagnostic cardiac ultrasound. Quick Facts
Why do people need an echo test? Your doctor may use an echo test to look at your heartís structure and check how well your heart functions. The test helps your doctor find out:
What are the risks?
How do I prepare for the echo? You donít have to do anything special. You can eat and drink before the test like you usually would. What happens during the echo? Echo test is done by specially trained technician. You will have your test done in our office. The test takes about half an hour.
What happens after the echo? Echo test is done by specially trained technician. You will have your test done in our office. The test takes about half an hour.
Back to Top STRESS TESTING What is an Exercise EKG Stress Test? A stress test, sometimes called a treadmill test or exercise test, helps a doctor find out how well your heart handles work. As your body works harder during the test, it requires more oxygen, so the heart must pump more blood. The test can show if the blood supply is reduced in the arteries that supply the heart. It also helps doctors know the kind and level of exercise appropriate for a patient. A person taking the test...
What is a Nuclear Stress Test with Exercise? In this test, the aim is to find out whether any areas of the heart muscle are not receiving enough blood flow during exercise. A radionuclide, is injected into a vein in the hand or arm. When the radionuclide has circulated through the blood stream, a gamma camera takes pictures of the heart while the patient is lying down. This is known as the "rest scan" of the heart. The patient then gets up and goes onto a treadmill. The treadmill starts off slowly and gradually picks up speed and incline so that the patient feels he is walking (or running) uphill. At peak exercise more radionuclide is injected into the patient. When the radionuclide has passed through the blood stream, the gamma camera takes more pictures of the heart. This is known as the "stress scan" of the heart. Computer system processes the resting and stress images which are then compared to assess for any lack of blood flow to any part of the heart muscle of the pumping chamber of the heart. The radionuclide helps blocked or partially blocked arteries show up on the scans, because they do not absorb the radionuclide into the heart - they are known as "cold spots". What is a Chemical Nuclear Stress Test without Exercise? Some patients, such as those with severe arthritis, are unable to do the physical activity required in a test with exercise. Instead, they are given medications that either speed up the heart rate or dilate the arteries. The body responds in a similar way it would to exercise. A radionuclide is injected into the patient's arm or hand while he/she is resting. When it has circulated through the bloodstream, a gamma camera takes pictures of the heart - during this process the patient is lying down motionless. As in the test with exercise, this is also known as the "rest scan" of the heart. The doctor then administers a medication to either speeds up the heart rate or dilates the arteries. When the peak heart rate is reached, the patient is injected again with a radionuclide. As soon as it has circulated throughout the bloodstream the gamma camera takes more pictures. This phase of the procedure is called the "stress scan" of the heart. Computer system processes the resting and stress images which are then compared to assess for any lack of blood flow to any part of the heart muscle of the pumping chamber of the heart. As in the stress test with exercise, blocked or partly blocked arteries will show up as "cold spots". Back to Top HOLTER MONITORING What is a Holter Monitor? A Holter monitor is a battery-operated portable device that measures and tape records your heartís activity EKG continuously for 24 to 48 hours or longer depending on the type of monitoring used. The device is the size of a small camera. It has wires with silver dollar-sized electrodes that attach to your skin. The Holter monitor and other devices that record your ECG as you go about your daily activities are called ambulatory electrocardiograms. Quick facts:
Why do people wear Holter Monitors? Regular electrocardiograms (ECGs or EKGs) let your doctor look at your heartís activity at one point in time during your ECG test. But abnormal heart rhythms and cardiac symptoms may come and go. Thatís why your doctor may want to evaluate your heartbeat over time while you go about your normal activities. You may be asked to wear a Holter monitor if you have fast, slow or irregular heartbeats called arrhythmias. What will wearing the monitor tell my doctor?
What are the risks of Holter Monitors? Wearing a Holter monitor has no risks and causes no pain. Holter monitors have wires that connect to small discs (electrodes) attached to your chest to record the electrocardiogram. Because the electrodes are attached with tape or adhesives, they may cause mild skin irritation. Tell the technician if you are allergic to any tapes or adhesives. What should I expect with the Holter Monitor? A specially trained technician will attach the Holter monitor and instruct you how to record your symptoms while wearing it.
What happens after wearing a Holter Monitor? After the test period, return the monitor to the technician. He or she will process the record of your heart activity and prepare a report for your doctor. This will include the notes in your diary. You should get the results of the test in one or two weeks. Back to Top CARDIAC CATHETERIZATION / ANGIOPLASTY / STENT 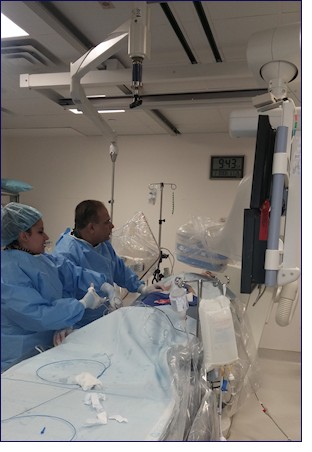 What is Cardiac Catheterization?
Cardiac catheterization is a procedure to examine how well your heart is working. A thin, hollow tube called a catheter is inserted into a large blood vessel that leads to your heart.
Quick facts:
What is Cardiac Catheterization?
Cardiac catheterization is a procedure to examine how well your heart is working. A thin, hollow tube called a catheter is inserted into a large blood vessel that leads to your heart.
Quick facts:
Why do people have cardiac catheterization? A cardiac cath provides information on how well your heart works, identifies problems and allows for procedures to open blocked arteries. For example, during cardiac cath your doctor may:
What are the risks of cardiac catheterization? Cardiac cath is usually very safe. A small number of people have minor problems. Some develop bruises where the catheter had been inserted (puncture site). The contrast dye that makes the arteries show up on X-rays causes some people to feel sick to their stomachs, get itchy or develop hives. How do I prepare for cardiac catheterization?
What happens during cardiac catheterization? A doctor with special training performs the procedure with a team of nurses and technicians. The procedure is done in a hospital cardiac catheterization (cath) lab.
What happens after cardiac catheterization? You will go to a recovery room for a few hours. During this time, you have to lie flat.
What happens after I get home? Be sure to carefully follow all instructions. It is important to take your medications as directed by your healthcare provider and to make follow up appointments before leaving the hospital. Most people can return to their normal activities the day after the procedure depending on whether any additional interventions were done during the cardiac cath. A small bruise at the puncture site is normal. If the site starts to bleed, lie flat and press firmly on top of it for a few minutes. Then, recheck to see if the bleeding has stopped. Call your doctor if:
Back to Top SCLEROTHERAPY Sclerotherapy is a medical procedure used to eliminate spider veins. Sclerotherapy involves an injection of a solution (generally polidocanol) directly into the vein. The solution irritates the lining of the vein, causing it to swell and stick together, and the blood to clot. Over time, the vessel turns into scar tissue that fades from view. Am I a candidate for Sclerotherapy? Prior to sclerotherapy, you will have an initial consultation with Dr Sahgal to decide if you're a good candidate for the procedure. Your eligibility will be decided on an individual basis, and will depend on the overall health of the area needing treatment. How is Sclerotherapy Done? In most cases of sclerotherapy, the medication solution is injected through a very fine needle directly into the vein. At this point, you may experience mild discomfort and cramping for one to two minutes, especially when larger veins are injected. The procedure itself takes approximately 15 to 30 minutes. The number of veins injected in one session depends on the size and location of the veins, as well as the general medical condition of the patient. Sclerotherapy is performed in our office by Dr Sahgal and requires that you do not do any aerobic activity for a few days after the procedure. What to Do Before Sclerotherapy? Prior to sclerotherapy, you should avoid certain anti inflammatory medications, such as Advil, Motrin, alleeve. Tylenol, however, should not affect this procedure. No lotion should be applied to the legs before the procedure. What are the side effects of Sclerotherapy You may experience certain side effects after sclerotherapy. There are milder effects, such as itching which can last for one or two days after the procedure. Also, you may experience raised, red areas at the injection site. These should disappear within a few days. Bruising may also occur around the injection site and can last several days or weeks. Are there any other side effects of Sclerotherapy
What happens after Sclerotherapy? After sclerotherapy you will be able to drive yourself home and resume your regular daily activities. Walking is encouraged. You will be instructed to wear support hosiery to "compress" the treated vessels. If you have compression hosiery from previous treatments, you are encouraged to bring them with you to be certain they still have adequate compression. Following the injections, avoid aspirin, ibuprofen, or other anti-inflammatory drugs for at least 48 hours. Tylenol may be used if needed. Also, you should avoid the following for 48 hours after treatment:
How effective is Sclerotherapy? Studies have shown that as many as 50%-80% of injected veins may be eliminated with each session of sclerotherapy. Less than 10% of the people who have sclerotherapy do not respond to the injections at all. In these instances, different solutions can be tried. Although this procedure works for most patients, there are no guarantees for success. In general, spider veins respond in three to six weeks, and larger veins respond in three to four months. If the veins respond to the treatment, they will not reappear. However, new veins may appear at the same rate as before. If needed, you may return for injections. Will my insurance cover Sclerotherapy? If your veins are causing medical problems such as pain or chronic swelling, your insurance may offer reimbursement. If sclerotherapy is being done for cosmetic purposes only, your carrier most likely will not provide coverage. If you have questions, call your insurance company, which may request a letter from us concerning the nature of your treatment and medical necessity. Back to Top VENEFIT (VNUS CLOSURE) PROCEDURE What is an Venefit (VNUS Closure) Procedure? The Venefit procedure, previously known as the VNUS Closure Procedure, offers patients an efficient, non-surgical alternative for treating varicose veins to improve the skinís appearance and to reduce health risks related to large varicose veins. The Venefit Procedure utilizes radiofrequency (RF) energy to heat and contract the collagen found inside the vein walls, causing the vein to collapse and seal shut. What are the advantages and benefits of the Venefit/VNUS Closure Procedure? 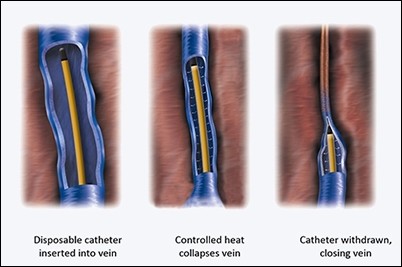
Before and After Venefit Closure Procedure 



Using ultrasound, your physician will position the Venefit catheter into the diseased vein through a small opening in the skin. The tiny radiofrequency powered catheter delivers heat to the vein wall. After sealing the vein, blood flow redirects to healthy veins, thus reducing or eliminating the appearance of enlarged, diseased veins. The Venefit procedure is performed on an outpatient basis and typically takes about 30 minutes. Local anesthesia is used for patient comfort. In some cases, this procedure is performed in conjunction with Ultrasound Guided Sclerotherapy or Ambulatory phlebectomy. Following the procedure, a simple bandage is placed over the insertion site, and additional compression may be provided to aid healing. Your doctor may encourage you to walk, and to refrain from extended standing and strenuous activities for a period of time. Patients who undergo the Venefit procedure typically resume normal activities within a day. How is the Venefit Procedure different from vein stripping? Vein stripping is an invasive surgical procedure that requires removing the vein through an incision during surgery. Vein stripping is typically performed in the operating room under full anesthesia. The Venefit Procedure, on the other hand, does not require surgery nor the removal of the vein. Instead, the vein is left in place and is closed using a special catheter inserted through a very small puncture. Instructions after your VNUS closure Procedure
What you may expect after your VNUS Closure Procedure: 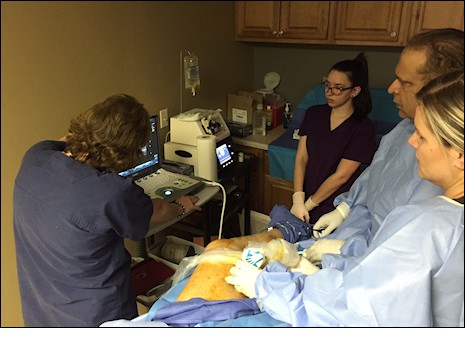 VNUS Closure procedure is a minimally invasive technique leaving almost no evidence of trauma or scaring at the skin surface, however there is a modest amount of trauma to the veins beneath the skin surface. The procedure works by heating the inner lining of the vein to just over the boiling point of water, causing the vein to coagulate and begin the process of slowly digesting away. You will experience no pain from this because the area is numbed by the local anesthesia.
Over next 3-6 hours, you should expect to begin to feel slight discomfort as anesthesia wears off. Most patients will feel better with over the counter pain medications (such as Ibuprophen). However, if you need something stronger, our office will call in a prescription for a stronger pain reliever. Most patients can return to normal activity within 24 to 48 hours with minimal discomfort. Although the pain is different, it is usually less than what you have long suffered with your venous disease which should begin to diminish almost immediately.
Over the next several days, you will begin to notice some swelling and minor tenderness along the course of the Ďclosed veiní. It is mildly tender to the touch and sometimes slightly bruised. Patients sometimes complain that it feels like something is pulling or stretching inside. This is entirely normal. The tenderness may take a month or more to fully resolve however the firm cord will take 4-6 months to slowly shrink and disappear. There may also be some mild numbness of the skin in the area of treatment. It too will almost always resolve itself, and may take up to a year.
If you have also had ultrasound or Veinlite guided injection sclerotherapy, this same phenomenon will occur although the firm Ďlumpsí will be more prominent because they are closer to the skin.
If you had phlebectomies, there will be small butterfly tapes over these small wounds. They may fall off in a few days. If not you can gently remove them if they remain on after 5 days.
Healing process that begins the day of the procedure, unfolds over a series of months. The relief of your original Ďvenous painí occurs quickly and is usually dramatic. The healing process from the Ďcoagulationí of the vein(s) however takes longer time. Any discomfort you may suffer will be very minor, and you should be back to full activities within a few days.
VNUS Closure procedure is a minimally invasive technique leaving almost no evidence of trauma or scaring at the skin surface, however there is a modest amount of trauma to the veins beneath the skin surface. The procedure works by heating the inner lining of the vein to just over the boiling point of water, causing the vein to coagulate and begin the process of slowly digesting away. You will experience no pain from this because the area is numbed by the local anesthesia.
Over next 3-6 hours, you should expect to begin to feel slight discomfort as anesthesia wears off. Most patients will feel better with over the counter pain medications (such as Ibuprophen). However, if you need something stronger, our office will call in a prescription for a stronger pain reliever. Most patients can return to normal activity within 24 to 48 hours with minimal discomfort. Although the pain is different, it is usually less than what you have long suffered with your venous disease which should begin to diminish almost immediately.
Over the next several days, you will begin to notice some swelling and minor tenderness along the course of the Ďclosed veiní. It is mildly tender to the touch and sometimes slightly bruised. Patients sometimes complain that it feels like something is pulling or stretching inside. This is entirely normal. The tenderness may take a month or more to fully resolve however the firm cord will take 4-6 months to slowly shrink and disappear. There may also be some mild numbness of the skin in the area of treatment. It too will almost always resolve itself, and may take up to a year.
If you have also had ultrasound or Veinlite guided injection sclerotherapy, this same phenomenon will occur although the firm Ďlumpsí will be more prominent because they are closer to the skin.
If you had phlebectomies, there will be small butterfly tapes over these small wounds. They may fall off in a few days. If not you can gently remove them if they remain on after 5 days.
Healing process that begins the day of the procedure, unfolds over a series of months. The relief of your original Ďvenous painí occurs quickly and is usually dramatic. The healing process from the Ďcoagulationí of the vein(s) however takes longer time. Any discomfort you may suffer will be very minor, and you should be back to full activities within a few days.Back to Top |

|
|
|
||
|
|
HOME PAGE | ABOUT US | SERVICES | PATIENT INFORMATION | CONTACT US |
|